
Get your ticket now for the live course in Rockville, MD on 11/3/19! The class will decrease test anxiety related to the pediatric CCRN exam, review test content, identify resources, and review practice questions with rationales.

Get your ticket now for the live course in Rockville, MD on 11/3/19! The class will decrease test anxiety related to the pediatric CCRN exam, review test content, identify resources, and review practice questions with rationales.
This study guide includes test content and more than 400 practice questions with rationales. Order yours today!
Check back to see the dates and locations of the live one day Pediatric CCRN Review Courses! These classes will review test content and test strategies.

The June 2019 Pediatric Care section of Critical Care Nurse features an article called Using Valid and Reliable Tools for Pain and Sedation Assessment in Pediatric Patients (Miller-Hoover, 2019), which discusses appropriate use of several different pain and sedation scales. Nurses must understand the scales used in their facilities and ensure that the proper scale is used for different scenarios to decrease the risk of adverse events, improve pain management, and meet regulatory standards.
Uses of the scales discussed include sedation, procedural sedation, mechanical ventilation, and pain. Age and developmental level of the child assists the nurse in choosing an appropriate scale. Assessment of delirium is vital in differentiating pain in an agitated patient who is verbally responsive. New standards from The Joint Commission’s Standard Revisions Related to Pain Assessment and Management in January 2018 include monitoring safe opioid prescribing oversight, assessing high-risk patients, collaborating pain goals with patients, creating more access to prescription drug monitoring programs, and creating competency validation focusing on increased safety and quality improvement.
Miller-Hoover, S.R. (2019). Using Valid and Reliable Tools for Pain and Sedation Assessment in Pediatric Patients. Critical Care Nurse, 39(3), 59-66.
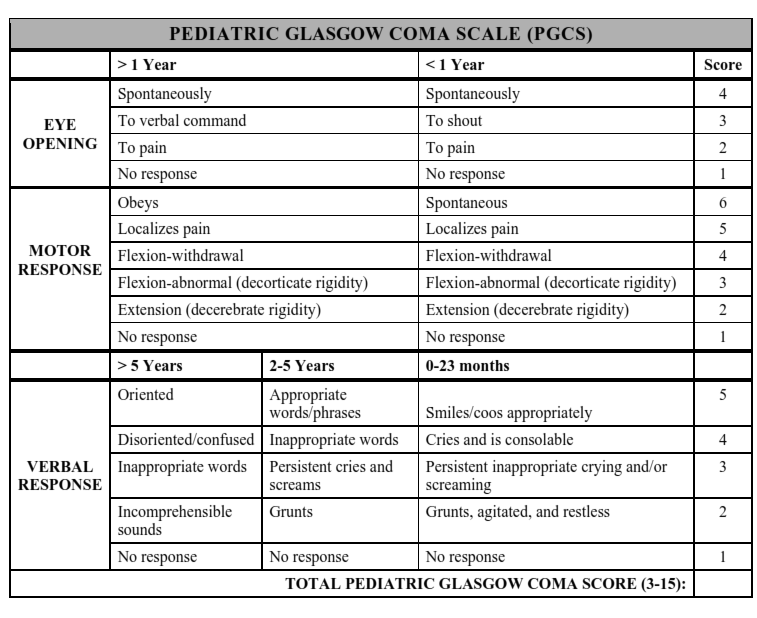
The June cover of Critical Care Nurse features an article on Routine Neurological Assessments by Nurses in the Pediatric Intensive Care Unit (Kirschen et al., 2019) which discusses a quality improvement intervention over a 1-year period. The goal was to standardize neurological assessments by nursing staff, improve the compliance of providers entering orders, improve nursing documentation, and assess the frequency of neurological decline before admission and after discharge. The study successfully improved ordering and documenting neurological assessments and found that patients with developmental disabilities were more likely to experience a decline in neurological status than patients who do not have a developmental disability.
How is this relevant to the pediatric CCRN exam? Clinical inquiry includes questioning the appropriateness of policies, guidelines, and current practices to continuously improve patient outcomes. Identifying and addressing differences in practice are important in clinical inquiry to ensure that best practices are followed. Standardization in ordering and documenting neurological assessments is important in identifying objective patient declines in order to intervene early and appropriately. While blood pressure, heart rate, and intracranial pressure are objective measures of neurological assessment, the use of the Glasgow Coma Scale may vary from nurse to nurse.
Clinical inquiry is a Professional Caring and Ethical Practice in the American Association of Critical Care Nurses (AACN) synergy model, which defines patient characteristics and nurse characteristics explaining how they can best be combined to improve outcomes. Professional Caring and Ethical Practice encompasses 20% (80 questions) of the pediatric CCRN exam.
Kirschen, M. P., Lourie, K., Snyder, M., Agarwal, K., DiDonato, P., Kraus, B., ...Topjian, A. (2019). Routine Neurological Assessments by Nurses in the Pediatric Intensive Care Unit. Critical Care Nurse, 39(3), 20-32.
Photo credit: http://boneandspine.com/wp-content/uploads/2013/08/pediatric-glsagow-coma-scale.png
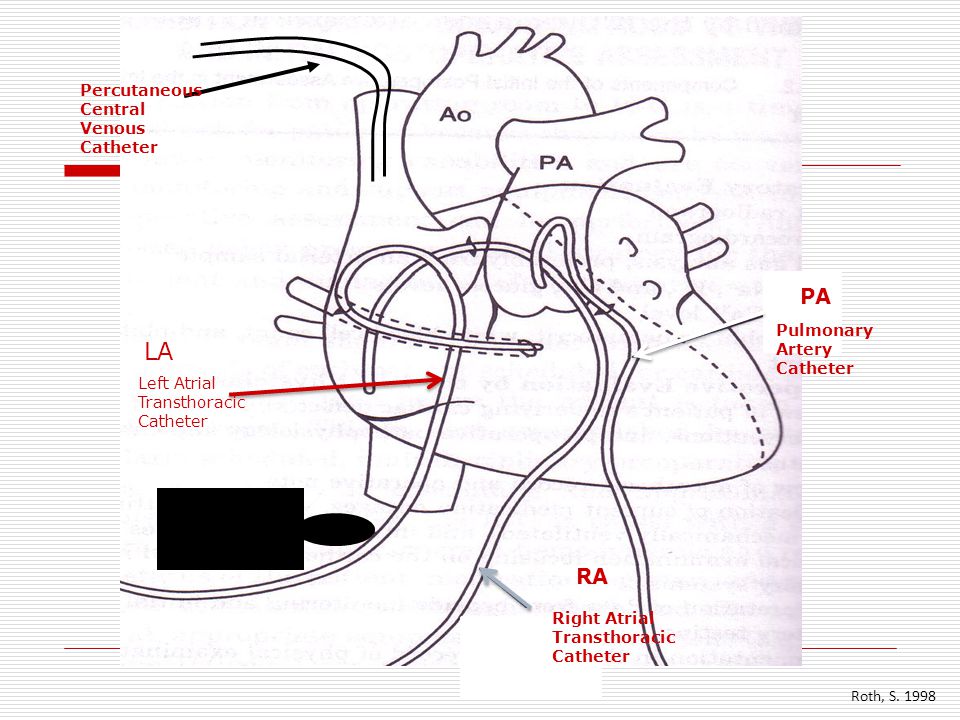
Transthoracic Intracardiac Catheters (TICs)
Nursing Practice with Transthoracic Intracardiac Catheters in Children: International Benchmarking Study (Lisanti, Fitzgerald, Helman, Dean, Sorbello, et al, 2019) is an article in the current 2019 issue of American Journal of Critical detailing a cross-sectional, descriptive study of nursing practice in infants and children with TICs seeking to define criteria for catheter insertion and removal, dressing care, flushing practice, securement, and mobilization of patients. Nurses participating in the study from 43 facilities (n=40) used TICs.
A review of the literature revealed that standard practices for management do not currently exist. The study of surveyed colleagues found that most institutions use TICs for blood administration and total parenteral nutrition (TPN). If the line was kept in greater than 5 days, it was more likely to be used for lab draws as well as blood product administration. Dressing changes are done every 7 days in 65% of the participating facilities. Unfortunately, only about half of the surveyed nurses reported that patients with TICs were mobilized out of bed.
The study was limited by reliance on self-reporting versus objective data. Ultimately, more research is needed to standardize management and improve outcomes.
Lisanti, A.J., Fitzgerald, J., Helman, S., Dean, S., Sorbello, S., & Griffis, H. (2019). Nursing Practice with Transthoracic Intracardiac Catheters in Children: International Benchmarking Study. American Journal of Critical 28(3). (174-181). Retrieved from doi:10.4037/ajcc2019350
Photo credit: https://slideplayer.com/slide/5339658/

The May 2019 issue of Bold Voices highlights 3 American Association of Critical Care Nurses (AACN) chapters who have implemented strategies to increase the number of certified nurses, increase the renewal and retention of certified nurse, influence the preparation or ability of nurses to qualify for certification, and increase public awareness and promote the value of certified nurses. These chapters include the AACN Dallas County chapter, the AACN Houston Gulf Coast chapter, and the AACN Greater Raleigh Area chapter. The article goes on to discuss activities at the 2019 National Teaching Institute & Critical Care Exposition (NTI).
What does this mean for nurses seeking pediatric CCRN certification? The article does not mention any certification review courses for this exam. In fact, the number of pediatric CCRN qualified candidates is who tested in 2018 (1.562) is much lower than the number of adult CCRN candidates (15,609).
While the number of adult intensive care units (ICUs) in the United States (US) is definitely higher than the number of pediatric intensive care units (PICUs), the number of PICUs is has grown in recent years. I believe that the number of pediatric CCRN candidates tested remains low due to a lack of resources. A quick Google search for adult CCRN review courses yields many options, while the results for searching for pediatric CCRN review courses is limited, and most do not offer flexibility or self-pacing.
Pediatric CCRN certification offers so much more to the learner than merely the addition of letters behind one’s name. The investment in certification can lead to an application to certified nurse anesthetist (CRNA) school, nurse practitioner (NP) school, and/or a promotion into a leadership or teaching role. And most importantly, it improves the outcomes of patients, which is the real reason we do what we do everyday.
https://www.aacn.org/certification/preparation-tools-and-handbooks/exam-stats-and-scores
http://www.nxtbook.com/nxtbooks/aacn/boldvoices_201905/index.php#/6
Photo credit: https://ww2.mc.vanderbilt.edu/nepd/44428

Are you going to NTI this year?! If so, congrats! The conference offers a wealth of information, networking, and inspiration. I am sad to say that I will be unable to attend at 34 weeks pregnant, but I wanted to ensure that anyone going has checked out the available resources! The May 2019 issue of Bold Voices has a great article called Top Tips for the Best NTI Experience found here → http://www.nxtbook.com/nxtbooks/aacn/boldvoices_201905/index.php#/4
You don’t want to get lost in the magnitude of the conference! The article suggests perusing the frequently asked questions page at www.aacn.org/nti, as well as using the My NTI tool to create a schedule and plan your week. Sunrise Sessions are available, but require a reservation. The NTI Program Planning Committee will be chairing “Navigating NTI 101” on Sunday, May 19 at 1615 or Monday, May 20 at 0800 to offer suggestions on how to make the experience the best for you. If you’re staying and making a vacation out of the conference, www.visitorlando.com highlights the amusement parks, cultural activities, and outdoor activities. And don’t miss the Nurses’ Night Off at Univeral Studios Florida on Wednesday, May 22 from 1930-2300! One complimentary ticket is included with your NTI registration.
If you get there early, it is recommended to tour and familiarize yourself with the convention center to maximize navigation of key places. Another tool provided on www.aacn.org/nti is the Learning Action Journal, which can also be found in your attendee bag. As with any conference, it is recommended to dress comfortably and to plan for either bringing your own or purching meals, snacks, and water for breaks throughout the day.
http://www.nxtbook.com/nxtbooks/aacn/boldvoices_201905/index.php#/4
Photo credit: https://meetingsource.com/sourcing-resource/destination-favorite-orlando-florida/
 Happy Nurse’s Week everyone!
Happy Nurse’s Week everyone!
This time of year (May 6th-12th) nurses are recognized nationally for their hard work, passion, and service. Plus there’s a lot of free stuff! This website https://gimmiefreebies.com/national-nurses-week-nurse-appreciation-week-freebies-deals/ lists fun freebies for nurses from a free 16 0z. Dunkin’ Dark Roast iced coffee May 6-12, between 4 p.m. and 10 p.m. with a valid health care ID to a free Cinnabon® Classic Cinnamon Roll, MiniBon®, or 4-count BonBites™ when nurses show their healthcare ID badge. While Chipotle is NOT offering their BOGO deal for nurses this year, participating Chipotles are offering medical professional BOGO 50% OFF every Wednesday!
So what about Pediatric CCRN Online Review? Nurses Week is coming early! Now through May 12th, we are offering $75 off our full online program with code NursesWeek2019 and $20 off our online practice questions with code NursesWeek2019Questions!
Nurses who invest in their careers will always benefit. Pediatric CCRN certification is often pursued by nurses before applying to CRNA, NP school, or a promotion. More importantly, certification improves the outcomes of our patients. And isn’t that why we became nurses?
Photo credit: https://gimmiefreebies.com/national-nurses-week-nurse-appreciation-week-freebies-deals/
Arteriovenous malformation (AVM) is an abnormal connection between the arteries and veins in the brain, making it the most common cause of intracranial hemorrhage in children. Treatment options include surgery, radiosurgery, and irradiation depending on the patient’s condition. Dilated pupils and nystagmus are not symptoms of AVM. Seizures are seen if the AVM has hemorrhaged.
AVM places patients at risk for hemorrhage and rebleeding after surgery. Signs and symptoms of hemorrhage include severe headache, seizures, decreased level of consciousness, hypotonia, irritability, decreased hemoglobin, and abnormal eye movements in a patient that is slowly deteriorating. Signs and symptoms in a rapidly deteriorating patient include coma, apnea, seizures, and unreactive pupils. Creating a calm environment keeps intracranial pressure (ICP) low and decreases vasospasm.
The cause of congenital neurologic abnormalities is unknown. A ventriculoperitoneal shunt may be indicated if hydrocephalus is present to decrease intracranial pressures. Nursing diagnoses include potential for infection after surgery, potential for decreased cardiac output related to anaphylactic shock from latex hypersensitivity, altered cerebral tissue perfusion related to increased ICP due to hydrocephalus, and altered elimination related to decreased innervation of bladder, urinary sphincter, and lower intestines.
Structure of the exam
The pediatric CCRN exam is 150 questions, 25 of which are used for statistical analysis for future tests. This equates to 125 questions that are scored. The exam lasts 3 hours and candidates receive their test results immediately if you take the computer based exam.
The test is divided into clinical judgment, which is 80% (120 questions) of the exam, and professional caring and ethical practice, which is 20% of the exam. Clinical judgment is further divided into cardiovascular (15% - 22.5 questions), pulmonary (16% - 24 questions), endocrine/hematology/gastrointestinal/renal/integumentary (19% - 28.5 questions), musculoskeletal/neurology/psychosocial (16% - 24 questions), and multisystem (14% - 21 questions).
Professional caring and ethical practice is the remaining 20%, or 30 questions. Professional caring and ethical practice is based on a model created by the American Association of Critical Care Nurses (AACN) called the Synergy Model. The Synergy model discusses a set of patient characteristics and a set of nurse characteristics.
Synergy occurs when the patient characteristics match the nurse characteristics. Patient characteristics include resiliency, vulnerability, stability, complexity, resource availability, participation in care, participation in decision making, and predictability. Nurse characteristics include clinical judgment, advocacy/moral agency, caring practices, response to diversity, facilitation of learning, collaboration, systems thinking, and clinical inquiry.
https://www.aacn.org/certification/preparation-tools-and-handbooks/~/media/aacn-website/certification/get-certified/handbooks/ccrnexamhandbook.pdf?la=en
Most states have determined that brain death guidelines for infants, children, and adults include one or two of the following conditions: 1. irreversible cessation of breathing and circulation OR 2. irreversible cessation of whole-brain functions (such as cortical or brainstem). The process in confirming brain death may vary from state to state. Presence of doll’s eyes and absence of a nystagmus with cold calorics indicates absence of oculocephalic and oculovestibular reflexes.
A normal oculovestibular reflex is seen when cold water is flushed into the ears causing nystagmus. Absence of this reflex is abnormal and may indicate brain death. A normal oculocephalic reflex is present when the head is rapidly turned to one side and the eyes deviate to the opposite side of head movement. Presence of doll’s eyes may be indicative of brain death. The time allowed following disconnection from the ventilator to allow PaCO2 to increase to stimulate a spontaneous breath is 5-10 minutes.
Brain death is part of the test plan under neurology. Musculoskeletal/Neurology/Psychology makes up 16% of the exam, which equals 24 questions.
Have you ever had a patient with a chest tube and you notice new continuous noisy or turbulent bubbling in the water seal chamber? A leak may be present, but first check that all connections are tight and secure. Clamp the chest tube at the insertion site (or closest to the dressing) using padded clamps and reassess the water chamber. If the bubbling stops, the leak is probably caused by patient air leak into the pleural space (in the lung) or at the insertion site. Unclamp immediately. Never clamp the chest tube for more than a few seconds or you risk a tension pneumothorax.
If the bubbling does not stop, reclamp the chest tube with padded clamps just a few inches distal to the insertion site and reassess the bubbling in the chamber to attempt to locate the air leak. Remember to only clamp the chest tube for a few seconds at a time. If the bubbling stops close when the chest tube is clamped close to a connection, you may be able to reseal the connection and fix the problem. If you clamp the system all the way from the patient to chamber and still have bubbling in the water seal chamber, the entire system may need to be changed.
Check out this video at 2:45 for visual demonstration: https://www.youtube.com/watch?v=Ui0eKmEk38M
Hazinski, M.F. (2013). Nursing Care of the Critically Ill Child. 3rd ed. St. Louis, MO: Mosby/Elsevier
In 2018, the American Association of Critical Care Nurses (AACN) released a new product for pediatric CCRN certification. The third edition of AACN Core Curriculum for Pediatric High Acuity, Progressive, and Critical Care Nursing is available on the AACN for $83 for members and $98 for non-members. The book was created as a tool for potential pediatric CCRN candidates.
Updates to the new edition include current patient management, updated drug information, a new chapter on professional nursing issues discussing quality, safety, communication, teamwork, work environment, and the ever popular current hot topic of personal wellness. The case studies have also been revised to reflect the latest version of the CCRN exam with questions and rationales. Amazon reviews report that the book is great, but it is very long and very detailed (which is very similar to the second edition).
Every person studies differently. Remember what worked for you in nursing school will likely work for you with this exam. The pediatric CCRN online review course provides over 500 practice questions with rationales, 6 hours of focused video content, a study guide, and a book containing concentrated test content and over 400 practice questions. This allows candidates to study at their own pace with maximum efficiency, which is ideal for nurses work 12 hour shifts.
AACN Core Curriculum for Pediatric High Acuity, Progressive, and Critical Care Nursing. 3rd ed. 2018. Slota M, ed. 968 pages.